After suffering an ischemic stroke, and only a short time after symptoms began, tPA may be used.
© Zerbor | Dreamstime
Patients who don't get to the hospital within 90 minutes of stroke symptoms starting may not be eligible to receive an effective 'clot-busting' drug called tPA. TPA quickly dissolves the clots that cause many strokes. Even when its clot-dissolving powers are removed, tPA can still protect brain cells in animals from the loss of oxygen and glucose induced by a stroke, Yepes' team reported in the Journal of Neuroscience (July 2012). 'We may have been giving the right medication, for the wrong reason,' Yepes says. 'tPA is more than a clot-busting drug.
When a blood clot is stopping blood flow to the brain, a powerful clot-busting medication called tPA is used to dissolve the clot and restore blood flow. The drug must be given within 4½ hours after the onset of symptoms, or the risk of causing unwanted bleeding may outweigh the benefit. The earlier tPA is administered within that time period, the better the chances of a favorable outcome.
Knowing a patient's vital signs, and armed with the results of a CT scan, ECG, blood tests, and history of stroke symptoms including time of onset, a physician can make a diagnosis. If the diagnosis is ischemic stroke, and only a short time has passed since symptoms began, tPA may be used.
Standard Treatment: tPA to Dissolve the Blood Clot
The technique for treating blood clots causing stroke is called intravenous thrombolysis—in lay terms, 'clot-busting.' Thrombolysis is the combination of two Greek words, 'thrombus,' meaning blood clot, and 'lysis,' meaning to dissolve or break apart. The body has a natural mechanism for doing this through proteins that circulate in the blood. One of these is plasminogen, an inactive protein that the body converts to plasmin, an enzyme that breaks apart and dissolves blood clots. To make this conversion, another enzyme called tissue plasminogen activator (tPA) is required.

Blood clotting is a dynamic process. Fibrin filaments act like nets to trap red blood cells and stop the bleeding. As fibrin filaments form, tPA in the serum of the trapped blood begins to adhere to the fibrin, converting plasminogen to plasmin. Plasmin attacks the fibrin filaments, dissolving the net and breaking up the blood clot.
Blood clots are broken apart by plasmin as they form. So long as there is sufficient stimulus for blood to clot, clots will form faster than plasmin can break them apart. When the stimulus vanishes, the blood clot eventually breaks apart and disappears. The objective of thrombolytic therapy is to accelerate the removal of a blood clot by enhancing the conversion of inactive plasminogen to clot-busting plasmin.
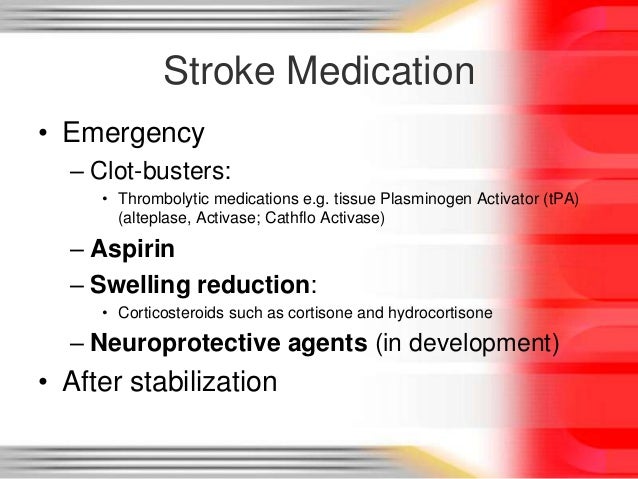
Emergency Medical Treatment for Stroke
The use of tPA is so effective in treating acute ischemic stroke that it is used in emergency departments throughout the country. Unfortunately, only about five percent of patients who qualify for the treatment receive it. One reason is failure to arrive at the hospital within the recommended treatment window of 4.5 hours.
While several tPA drugs can be used to break up heart attack-causing blood clots in the coronary arteries, only one is approved for the treatment of ischemic stroke: alteplase (Activase). It is given by intravenous infusion. About 10 percent of the entire dose is given at one time (bolus), with the remaining 90 percent infused over an hour.
Initially, it was thought alteplase had to be administered within three hours of stroke onset. But when clinical trials showed the drug was safe and effective for a longer period of time, the American Heart Association/American Stroke Association (AHA/ASA) endorsed expanding the treatment window to 4.5 hours. The drug label says that risks are increased when the drug is used in patients over age 75, and its effectiveness in those over age 80 has not been established. But in 2015, the AHA/ASA gave a positive recommendation to tPA use in older patients, acknowledging that risk may be increased, but that it does not outweigh the potential benefit in increasing the likelihood of remaining independent three months after a stroke.
The AHA/ASA continues to emphasize that results are better when patients are treated earlier. Patients who receive the therapy within 90 minutes have a better outcome than those who receive it later, even if within the allowed time period. For every 30 minutes that pass before blood flow is restored through a blocked artery, the probability of a good recovery drops by about 10 percent.
Know the Risks
A danger of thrombolytic therapy is the possibility of unwanted bleeding. Clot-busting drugs cannot tell the difference between a 'bad' clot that prevents blood flow to the brain cells and a 'good' clot that has been formed to stop blood flow from a ruptured intracranial artery. If the drug breaks down a good clot, a hemorrhagic stroke can occur. Despite careful dosing, intracranial hemorrhage occurs in some patients who receive alteplase. Nevertheless, in appropriately selected patients, the benefits far outweigh this potential complication.
When It's Too Late for tPA
For patients diagnosed with ischemic stroke after the treatment window has passed, no medication to restore blood flow has been proven effective. However, some of these patients may benefit from mechanical removal of the clot with a catheter-based device up to six hours after stroke onset.
The treatment for blood clots in the lungs depends on the severity of symptoms. Blood clots in the lungs are also called pulmonary embolisms. In the last 15 years, I have personally treated hundreds of patients hospitalized with blood clots in their lungs. I am writing this article based on my experience as well as a thorough review of medical literature.
Before reading this article, I suggest you read 'symptoms of blood clot in the lungs.' Once you understand the different types and severities of the symptoms, you will better understand the treatment options.
Unlike large corporate medical websites, I will not simply tell you about all the different medications and procedures that are available to treat blood clots in the lungs. I will tell you who needs what kind of treatment based on the severity and specifics of the situation. You can use this information to work with your doctor and better understand your treatment options.
Here are the specific situations we will explore:
- A cardiac arrest due to blood clots in the lungs
- Blood clots in the lungs with low blood pressure
- Large blood clots in the lungs blocking major arteries
- Multiple blood clots in the lungs with stable vital signs
- Small blood clots in the lungs
- Blood clots in the lungs during pregnancy
- Blood clot in the lungs with cancer
Treatments for a cardiac arrest due to blood clots in the lungs
As you already know from reading the article on symptoms of blood clots in the lungs, cardiac arrests are one of the symptoms of a blood clot. Unfortunately, many people with a pulmonary embolism die before they can get to a hospital.
The most important treatment for people that suddenly collapse due to a blood clot in the lungs is to start CPR right away. If you are CPR certified or know how to do CPR, you should start it as soon as possible, and have someone call 911. If you can find someone nearby who can perform CPR, you should tell that person to start CPR and then call 911 yourself.
The picture above shows how CPR can save someone in cardiac arrest due to a blood clot in the lungs. A sudden cardiac arrest happens with a pulmonary embolism when blood flow to the lungs is completely or almost completely blocked by the clot. When repeated chest compressions are performed with CPR, the force of the chest movement may push the clot out, and it may slide forward, creating an opening for blood to start flowing again. This blood flow may sustain life until the patient can be transported to the nearest emergency department and more advanced treatment can be started.
Blood clotting is a dynamic process. Fibrin filaments act like nets to trap red blood cells and stop the bleeding. As fibrin filaments form, tPA in the serum of the trapped blood begins to adhere to the fibrin, converting plasminogen to plasmin. Plasmin attacks the fibrin filaments, dissolving the net and breaking up the blood clot.
Blood clots are broken apart by plasmin as they form. So long as there is sufficient stimulus for blood to clot, clots will form faster than plasmin can break them apart. When the stimulus vanishes, the blood clot eventually breaks apart and disappears. The objective of thrombolytic therapy is to accelerate the removal of a blood clot by enhancing the conversion of inactive plasminogen to clot-busting plasmin.
Emergency Medical Treatment for Stroke
The use of tPA is so effective in treating acute ischemic stroke that it is used in emergency departments throughout the country. Unfortunately, only about five percent of patients who qualify for the treatment receive it. One reason is failure to arrive at the hospital within the recommended treatment window of 4.5 hours.
While several tPA drugs can be used to break up heart attack-causing blood clots in the coronary arteries, only one is approved for the treatment of ischemic stroke: alteplase (Activase). It is given by intravenous infusion. About 10 percent of the entire dose is given at one time (bolus), with the remaining 90 percent infused over an hour.
Initially, it was thought alteplase had to be administered within three hours of stroke onset. But when clinical trials showed the drug was safe and effective for a longer period of time, the American Heart Association/American Stroke Association (AHA/ASA) endorsed expanding the treatment window to 4.5 hours. The drug label says that risks are increased when the drug is used in patients over age 75, and its effectiveness in those over age 80 has not been established. But in 2015, the AHA/ASA gave a positive recommendation to tPA use in older patients, acknowledging that risk may be increased, but that it does not outweigh the potential benefit in increasing the likelihood of remaining independent three months after a stroke.
The AHA/ASA continues to emphasize that results are better when patients are treated earlier. Patients who receive the therapy within 90 minutes have a better outcome than those who receive it later, even if within the allowed time period. For every 30 minutes that pass before blood flow is restored through a blocked artery, the probability of a good recovery drops by about 10 percent.
Know the Risks
A danger of thrombolytic therapy is the possibility of unwanted bleeding. Clot-busting drugs cannot tell the difference between a 'bad' clot that prevents blood flow to the brain cells and a 'good' clot that has been formed to stop blood flow from a ruptured intracranial artery. If the drug breaks down a good clot, a hemorrhagic stroke can occur. Despite careful dosing, intracranial hemorrhage occurs in some patients who receive alteplase. Nevertheless, in appropriately selected patients, the benefits far outweigh this potential complication.
When It's Too Late for tPA
For patients diagnosed with ischemic stroke after the treatment window has passed, no medication to restore blood flow has been proven effective. However, some of these patients may benefit from mechanical removal of the clot with a catheter-based device up to six hours after stroke onset.
The treatment for blood clots in the lungs depends on the severity of symptoms. Blood clots in the lungs are also called pulmonary embolisms. In the last 15 years, I have personally treated hundreds of patients hospitalized with blood clots in their lungs. I am writing this article based on my experience as well as a thorough review of medical literature.
Before reading this article, I suggest you read 'symptoms of blood clot in the lungs.' Once you understand the different types and severities of the symptoms, you will better understand the treatment options.
Unlike large corporate medical websites, I will not simply tell you about all the different medications and procedures that are available to treat blood clots in the lungs. I will tell you who needs what kind of treatment based on the severity and specifics of the situation. You can use this information to work with your doctor and better understand your treatment options.
Here are the specific situations we will explore:
- A cardiac arrest due to blood clots in the lungs
- Blood clots in the lungs with low blood pressure
- Large blood clots in the lungs blocking major arteries
- Multiple blood clots in the lungs with stable vital signs
- Small blood clots in the lungs
- Blood clots in the lungs during pregnancy
- Blood clot in the lungs with cancer
Treatments for a cardiac arrest due to blood clots in the lungs
As you already know from reading the article on symptoms of blood clots in the lungs, cardiac arrests are one of the symptoms of a blood clot. Unfortunately, many people with a pulmonary embolism die before they can get to a hospital.
The most important treatment for people that suddenly collapse due to a blood clot in the lungs is to start CPR right away. If you are CPR certified or know how to do CPR, you should start it as soon as possible, and have someone call 911. If you can find someone nearby who can perform CPR, you should tell that person to start CPR and then call 911 yourself.
The picture above shows how CPR can save someone in cardiac arrest due to a blood clot in the lungs. A sudden cardiac arrest happens with a pulmonary embolism when blood flow to the lungs is completely or almost completely blocked by the clot. When repeated chest compressions are performed with CPR, the force of the chest movement may push the clot out, and it may slide forward, creating an opening for blood to start flowing again. This blood flow may sustain life until the patient can be transported to the nearest emergency department and more advanced treatment can be started.
Learning basic CPR is something anyone can do, and it only requires a day or two of training. Classes are offered in many places, including local hospitals, and you don't need any prior medical knowledge. Even many high schools have begun teaching CPR as part of a class. You may help save the life of someone in cardiac arrest if you learn this simple skill.
In people with major blood clots in the lungs leading to cardiac arrest, quick CPR is the most important treatment that makes a difference between life and death.
Treatments for blood clots in the lungs with low blood pressure
Low blood pressure with a blood clot in the lungs is an ominous sign. It means that the blood clot is blocking significant amounts of blood from going into your pulmonary artery. The situation is similar to what you saw in the first picture, except that there is barely enough blood flow to prevent a sudden collapse. Low blood pressure is a sign that the body is going into major shock, and may collapse anytime.
The first step in treating these people is to make sure they have stable breathing and blood circulation. If they are having trouble breathing, they need to have a tube placed in their airway and be connected to a ventilator. They will also need IV fluids to try to raise blood pressure. Medications may be necessary to squeeze the heart and the blood vessels in order to raise blood pressure.
While the life-supporting treatment is ongoing, doctors will also be making plans for a proper diagnosis and the next step in treatment, a CT scan of the chest. Slot machines for sale pa. It will help doctors see the blood clot and confirm the diagnosis.
Once the diagnosis is confirmed, treatment should be started right away. There are a few options for treatment. Small community hospitals or rural hospitals may not have all of the advanced options available.
Clot-busting medications
This is the first option used in the majority of these situations. Clot-busting medications are designed to dissolve blood clots. These are different from blood thinners, which we will learn about later. A commonly-used medication is called tissue plasminogen activator, or TPA. It is the same medication used in the treatment of strokes. There is a high risk because it can cause major life-threatening bleeding, but the benefits definitely outweigh the risks for most people.
The medication is infused through an IV line. The goal is to try to dissolve the clot so that blood starts flowing again.
Catheter guided treatment
This may be used as the first option in places where specialists that perform this procedure are immediately available. If the patient is unstable and it would take some time for the specialist to come to the hospital, it is better to get started with clot-busting medications. If the patient is relative stable, it may be worth waiting a little to start with catheter guided treatments than an IV TPA infusion. That is a judgement call made by the treating doctor.
Sometimes, catheter guided treatments are simply guiding a small tube under an x-ray to the site of the blood clot, and infusing TPA directly at the clot. This could more slightly more effective, and it may have a slightly lower risk of bleeding at other places.
Catheter guided treatments may also involve using small mechanical equipment attached to the tip of the catheter that can cut through the clot. Clot fragments are then suctioned away. This is a good option if a skilled specialist capable of doing such a procedure is available at the hospital.
Catheter guided treatments are also the second step used in people who did not have success with the IV TPA treatment.
Tpa Clot Busting Drug
Open surgery to remove the clot
Sometimes, it becomes necessary to perform open surgery to remove the clot. This surgery also requires highly-skilled specialized surgeons called cardiothoracic surgeons. The risk is high, but it could the only option to try and save the life of someone with blood clots in the lungs.
Infusion of blood thinners
A blood thinner called heparin is infused in all patients with life-threatening blood clots in the lungs, regardless of which of the above treatment options are used. Treatment is started as soon as blood clots in the lungs are suspected or confirmed. Heparin is used unless there is any specific problem in someone that prohibits its use. Unlike TPA, heparin is simply a blood thinner. Blood thinners prevent the formation of new clots. They weaken the clot-forming mechanism in our bodies, but do not directly dissolve the clots. The main goal of infusing heparin is to prevent new clots or an extension of an existing clot.
Treatments for large blood clots in the lungs blocking major arteries
Sometimes, you can have normal blood pressure, but still have large blood clots in the lungs blocking multiple major branches of the pulmonary artery, as seen in this picture. If your blood pressure is low, you will get the exact same treatment we discussed earlier. However, if you have large blood clots but a normal blood pressure, you may not need all of those high-risk treatments.
You still need to get started on heparin like we discussed earlier. After that, if your blood pressure is still stable, most doctors simply decide to watch you closely in the hospital. They will monitor your blood pressure closely during the hospital stay. If your blood pressure drops, you will get the more invasive treatments. If your blood pressure remain stable, you may only need blood thinners.
Some places may still offer you catheter guided treatments for large clots even when your blood pressure is fine. That is an important and individualized decision you need to make with your doctor after discussing the risks and benefits.
Treatments for multiple blood clots in the lungs with stable vital signs
These are the most common types of blood clots seen in the lungs of hospitalized patients. Fortunately, these patients have a relatively good outcome, and treatment is also straightforward. If you are hospitalized to a regular medical floor with blood clots in your lungs, you most likely have this type of pulmonary embolism.
As you can see in the picture, these clots don't significantly obstruct blood flow. You may have some chest or back pain, and you may need some oxygen to help you breathe.
The most commonly used blood thinner to treat this type of blood clot is an injection called low molecular weight heparin (LMWH). Most people know it by its brand name Lovenox. LMWH starts working right away, and most doctors prefer to use it in this type of blood clot.
During your hospital stay for this type of blood clot, you will most likely have an EKG and an ultrasound of your heart done to make sure that the right side of your heart is doing well with the clot. You may need further treatment if the right side seems to be struggling to push blood through the clot. Otherwise, they will monitor your blood pressure and oxygen levels. If your oxygen remains low, you may need oxygen treatments at home.
Before going home, you will be given treatment options for blood thinners. The tried and true medication that has been used for many years is called Warfarin. It is relatively inexpensive, but it needs frequent blood tests to adjust the dose. There are newer and more expensive blood thinners that don't need frequent blood tests. Examples of such medications include Rivaroxaban (brand name Xarelto), Apixaban (brand name Eliquis), and Dabigatran (brand name Pradaxa). These are all similar to Warfarin as far as effectiveness goes. The choice is personal. You need to make the right decision for yourself after talking to your doctor.
Treatments for small blood clots in the lungs
As you can see, small blood clots in the lungs don't block the flow of blood, but they may still cause chest or back pain. You don't necessarily need to be hospitalized with these types of blood clots. If your vitals are stable and if you are breathing normally without any extra oxygen, you can be discharged home from the emergency department or doctor's office.
Most doctors prefer to use newer blood thinners in these patients if they are going home instead of staying in the hospital. They are more convenient than Warfarin in these situations, because they start working relatively faster and don't need blood tests to monitor.
Treatments for blood clots in the lungs during pregnancy
The only difference in treating pregnant women with blood clots in the lungs is that warfarin or newer blood thinners are not safe to use during pregnancy. For the treatment of blood clots at home, pregnant women need to give themselves the LMWH injections.
Treatments for blood clots in the lungs with cancer
If you are being treated for cancer, your risk for getting blood clots goes up. They have done comparison studies in cancer patients and have found that LMWH injections work better than other blood thinners to prevent further clots in people with cancer. Most doctors prescribe LMWH for the treatment of blood clots in lungs with cancer.
Tpa Medication Stroke
I hope you have a clear understanding of treatments for blood clots in the lungs after reading this article. It is our attempt to put together the most comprehensive article on treatments for blood clots in the lungs that anyone can understand. After reading this article, if you still have any questions or doubts, please go to our ['LinkContact Us'Link] page and send us an email. We will update the article, including additional information that may be helpful to our readers. Remember, we will not answer any specific medical questions, but we will be happy to include any new informational topics that may be valuable to our readers.
Tpa Clot Buster Medication
References:
